It is time to start facing facts. There is no test that can yet prove your immunity to the novel coronavirus that causes COVID-19. Any talk of restarting tourism, or for that matter a return to how life was before the outbreak, using so-called “immunity passports”, should be seen as little more than wishful thinking at this stage. We will get there, but we should be clear, unless there is a major breakthrough, that can be verified and replicated in record time, the “new normal” is something we are going to have to adapt to and is as of yet an unwritten page in our history.
When we first started releasing information on the Coronavirus threat we were attacked from many quarters, painting us as “alarmist” or “scaremongering”, however our data analysis has so far proven to be more than accurate. In fact we have been perhaps a little too conservative. Now that everyone is a little more up to speed, we thought we would explore just some of our findings, backed up by the latest news from the World Health Organisation. We hope you will forgive the brutal nature of what we have to say.
What does any of this mean for the future of tourism and The Canary Islands? No-one yet knows, but it is plain to see that there will almost certainly be no restart of tourism this summer, and it is very likely that any relaxation of travel restrictions will need to be very closely monitored and controlled, as each visitor brings with them the potential to start a second wave of infection to, as far as we know, our largely uninfected population. Canary Islands ministers have already announced that visitor numbers this year will have dropped by the end of 2020 from the expected 16 million holiday makers to less than 3 million, most of whom already visited us in the first quarter of this year. Welcome to the “New Normal”.
 Many people, governments and other institutions around the world have spoken in recent weeks about the possible development of “Immunity Passports” as a way to try and certify whether or not individuals might be able to travel and resume “normal” activities again, having had the COVID-19 virus and developed immunity to getting it again. The simple fact, say the World Health Organisation (WHO), is that there is no reliable test anywhere yet that can categorically prove that once you have had the virus, you will not catch it again.
Many people, governments and other institutions around the world have spoken in recent weeks about the possible development of “Immunity Passports” as a way to try and certify whether or not individuals might be able to travel and resume “normal” activities again, having had the COVID-19 virus and developed immunity to getting it again. The simple fact, say the World Health Organisation (WHO), is that there is no reliable test anywhere yet that can categorically prove that once you have had the virus, you will not catch it again.
As Spain, and The Canary Islands, enter their 7th week of enforced “lockdown” and social distancing measures it is becoming ever more clear that there is little likelihood of any return to “normality” any time soon, or even before the end of 2020. Our most pressing issue right now is how we can protect ourselves and each other from second wave and third wave outbreaks, how we can manage that probability and continue to help our healthcare systems from being over run in the face of the persistent likelihood that this will not be under control for many months to come, perhaps even years.
 In a report, released this morning, the WHO have categorically stated that, despite the many efforts continuing around the world to develop a so-called “antibody test” to prove one way or another whether a person has had the virus and developed immunity, no such reliable test currently exists to indicate whether a person can still catch COVID-19 having already had it or whether or not they might be a carrier still able to infect others.
In a report, released this morning, the WHO have categorically stated that, despite the many efforts continuing around the world to develop a so-called “antibody test” to prove one way or another whether a person has had the virus and developed immunity, no such reliable test currently exists to indicate whether a person can still catch COVID-19 having already had it or whether or not they might be a carrier still able to infect others.
Regardless of the protestations of The Canary Islands Regional Government, coronavirus is here and with us to stay for the foreseeable future. The Canary Islands have tried to argue in recent days that they need to start relaxing movement restrictions early so as to save the tourism industry, however Spain has firmly resisted saying that all Spanish territories will remain under the same guidance, with economic activities suspended and almost total restrictions on travel, until there is clear evidence that the population can be brought out of “lockdown” together and with a reasonable degree of safety.
 Though many will throw their hands up in despair at this difficult news, the simple truth is that despite being one of the regions in Spain with the lowest rates of infection, in the main due to everyone’s diligence in observing the restrictions and complying with government advice quickly, the Autonomous Community of The Canary Islands will suffer some of the harshest effects of the global downturn, due to estimates of more than 35% of GDP having already been wiped off the books for this year, with a more than 80% drop in revenues in the tourism industry, and already a forecasted loss of more than a quarter of a million jobs, accounting for well over 12% of the population likely to be out of work, added to the already highest unemployment rate in Europe, meaning likely more than half of our population could cease to have any form of income whatsoever, until the economy can start to recover. And simply put, that is unlikely happen any time soon.
Though many will throw their hands up in despair at this difficult news, the simple truth is that despite being one of the regions in Spain with the lowest rates of infection, in the main due to everyone’s diligence in observing the restrictions and complying with government advice quickly, the Autonomous Community of The Canary Islands will suffer some of the harshest effects of the global downturn, due to estimates of more than 35% of GDP having already been wiped off the books for this year, with a more than 80% drop in revenues in the tourism industry, and already a forecasted loss of more than a quarter of a million jobs, accounting for well over 12% of the population likely to be out of work, added to the already highest unemployment rate in Europe, meaning likely more than half of our population could cease to have any form of income whatsoever, until the economy can start to recover. And simply put, that is unlikely happen any time soon.
What’s more, due to our comparative success in stopping the virus from ravaging our communities, we are largely thought to be an uninfected population. Which means we are still most susceptible to becoming infected by those with the virus at some point in the future. Though there is some possibility that many have already had the virus, we simply do not know. As the WHO have starkly said this morning, even if we have already had it, we currently have no way of knowing if we can get it again, nor who might still be infectious even if they have presented no symptoms whatsoever.
This is difficult news. Many will angrily respond to the ideas expressed here. There is absolutely no intention to sensationalise the situation. Those that speak of these things without clear knowledge are of no use whatsoever to any of us. The only way we are going to come through any of this with some semblance of our humanity is by calmly learning to adapt to what is still an evolving situation, helping those we can, protecting what is left, working together and developing a real sense of what is going to be most important to each of us moving forward. With much luck, perseverance and hard work we will rise above all these things as the “new normal” begins to emerge. But for now we must relax any insistence on attempts to too quickly return to how things were before. That time is behind us for the moment, we have a long road ahead.
Scientific Brief
https://www.who.int/news-room/commentaries/detail/immunity-passports-in-the-context-of-covid-19
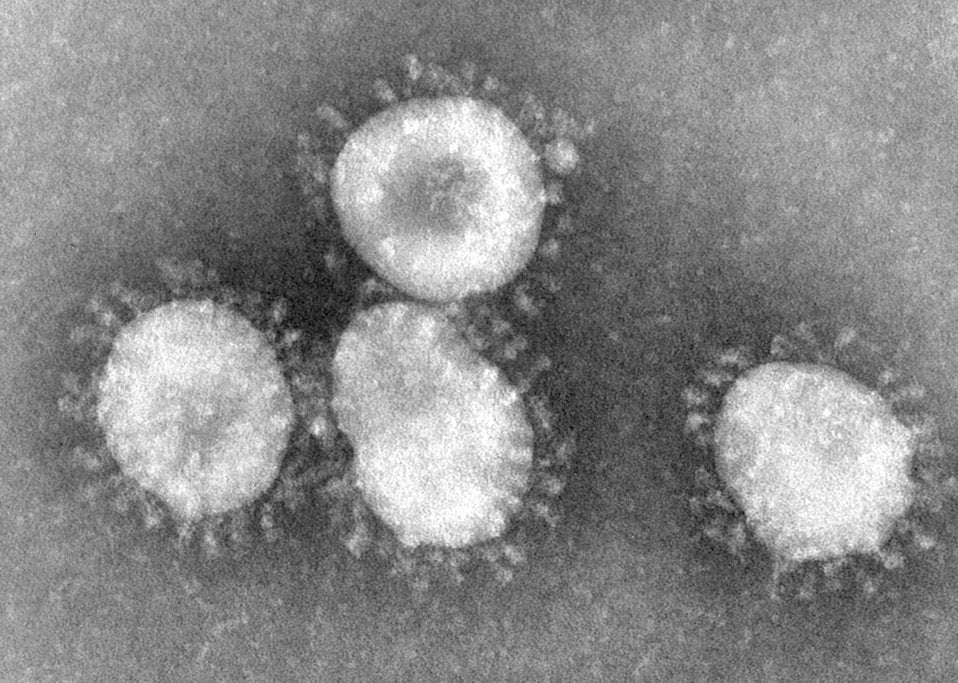
WHO has published guidance on adjusting public health and social measures for the next phase of the COVID-19 response.(1) Some governments have suggested that the detection of antibodies to the SARS-CoV-2, the virus that causes COVID-19, could serve as the basis for an “immunity passport” or “risk-free certificate” that would enable individuals to travel or to return to work assuming that they are protected against re-infection. There is currently no evidence that people who have recovered from COVID-19 and have antibodies are protected from a second infection.
The measurement of antibodies specific to COVID-19
The development of immunity to a pathogen through natural infection is a multi-step process that typically takes place over 1-2 weeks. The body responds to a viral infection immediately with a non-specific innate response in which macrophages, neutrophils, and dendritic cells slow the progress of virus and may even prevent it from causing symptoms. This non-specific response is followed by an adaptive response where the body makes antibodies that specifically bind to the virus. These antibodies are proteins called immunoglobulins. The body also makes T-cells that recognize and eliminate other cells infected with the virus. This is called cellular immunity. This combined adaptive response may clear the virus from the body, and if the response is strong enough, may prevent progression to severe illness or re-infection by the same virus. This process is often measured by the presence of antibodies in blood.
WHO continues to review the evidence on antibody responses to SARS-CoV-2 infection.(2-17) Most of these studies show that people who have recovered from infection have antibodies to the virus. However, some of these people have very low levels of neutralizing antibodies in their blood,4 suggesting that cellular immunity may also be critical for recovery. As of 24 April 2020, no study has evaluated whether the presence of antibodies to SARS-CoV-2 confers immunity to subsequent infection by this virus in humans.
Laboratory tests that detect antibodies to SARS-CoV-2 in people, including rapid immunodiagnostic tests, need further validation to determine their accuracy and reliability. Inaccurate immunodiagnostic tests may falsely categorize people in two ways. The first is that they may falsely label people who have been infected as negative, and the second is that people who have not been infected are falsely labelled as positive. Both errors have serious consequences and will affect control efforts. These tests also need to accurately distinguish between past infections from SARS-CoV-2 and those caused by the known set of six human coronaviruses. Four of these viruses cause the common cold and circulate widely. The remaining two are the viruses that cause Middle East Respiratory Syndrome and Severe Acute Respiratory Syndrome. People infected by any one of these viruses may produce antibodies that cross-react with antibodies produced in response to infection with SARS-CoV-2.
Many countries are now testing for SARS-CoV-2 antibodies at the population level or in specific groups, such as health workers, close contacts of known cases, or within households.(21) WHO supports these studies, as they are critical for understanding the extent of – and risk factors associated with – infection. These studies will provide data on the percentage of people with detectable COVID-19 antibodies, but most are not designed to determine whether those people are immune to secondary infections.
Other considerations
At this point in the pandemic, there is not enough evidence about the effectiveness of antibody-mediated immunity to guarantee the accuracy of an “immunity passport” or “risk-free certificate.” People who assume that they are immune to a second infection because they have received a positive test result may ignore public health advice. The use of such certificates may therefore increase the risks of continued transmission. As new evidence becomes available, WHO will update this scientific brief.
References
- Considerations in adjusting public health and social measures in the context of COVID-19. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/critical-preparedness-readiness-and-response-actions-for-covid-19
- Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature 2020.
- To KK, Tsang OT, Leung WS, et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020 Mar 23. pii: S1473-3099(20)30196-1. doi: 10.1016/S1473-3099(20)30196-1.
- Wu F, Wang A, Liu M, et al. Neutralizing antibody responses to SARS-CoV-2 in a COVID-19 recovered patient cohort and their implications. medRxiv 2020: 2020.03.30.20047365.
- Ju B, Zhang Q, Ge X, et al. Potent human neutralizing antibodies elicited by SARS-CoV-2 infection. Biorxiv 2020: 2020.03.21.990770.
- Poh CM, Carissimo G, Wang B, et al. Potent neutralizing antibodies in the sera of convalescent COVID-19 patients are directed against conserved linear epitopes on the SARS-CoV-2 spike protein. Biorxiv 2020: 2020.03.30.015461.
- Zhang W, Du R, Li B, Zheng X, et al. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020 Feb 17; 9(1):386-389. doi: 10.1080/22221751.2020.1729071.
- Grzelak L, Temmam L, Planchais C, et al. SARS-CoV-2 serological analysis of COVID-19 hospitalized patients, pauci-symptomatic individuals and blood donors. medRxiv 2020 (submitted 17 April 2020).
- Amanat F, Nguyen T, Chromikova V, et al. A serological assay to detect SARS-CoV-2 seroconversion in humans. medRxiv 2020: 2020.03.17.20037713.
- Okba NMA, Müller MA, Li W, et al. Severe acute respiratory syndrome coronavirus 2−specific antibody responses in coronavirus disease 2019 patients. Emerg Infect Dis. 2020 doi: 10.3201/eid2607.200841
- Zhao J, Yuan Q, Wang H, et al. Antibody responses to SARS-CoV-2 in patients of novel coronavirus disease 2019. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa344
- Guo L, Ren L, Yang S, et al. Profiling Early Humoral Response to Diagnose Novel Coronavirus Disease (COVID-19). Clin Infect Dis. 2020 Mar 21. doi: 10.1093/cid/ciaa310.
- Liu Y, Liu Y, Diao B, Ren Feifei, et al. Diagnostic indexes of a rapid IgG/IgM combined antibody test for SARS-CoV-2. medRxiv 2020; doi: 10.1101/2020.03.26.20044883
- Zhang P, Gao Q, Wang T, Ke Y, et al. Evaluation of recombinant nucleocapsid and spie protein serological diagnosis of novel coronavirus disease 2019 (COVID-19). medRxiv. 2020; doi: 10.1101/2020.03.17.20036954
- Pan Y, Li X, Yang G, Fan J, et al. Serological immunochromatographic approach in diagnosis with SARS-CoV-2 infected COVID-19 patients. medRxiv. 2020; doi: 10.1101/2020.03.13.20035428
- Li Z, Yi Y, Luo X, Xion N, et al. Development and clinical application of a rapid IgM-IgG combined antibody test for SARS-CoV-2 infection diagnosis. J Med Virol. 2020 Feb 27. doi: 10.1002/jmv.25727.
- Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2). Science 2020.
- Lou B, Li T, Zheng S, Su Y, Li Z, Liu W, et al. Serology characteristics of SARS-CoV-2 infection since the exposure and post symptoms onset. medRxiv 2020; doi: 10.1101/2020.03.23.20041707
- Lin D, Liu L, Zhang M, Hu Y, et al. Evaluation of serological tests in the diagnosis of 2019 novel coronavirus (SARS-CoV-2) infections during the COVID-19 outbreak. medRxiv 2020. doi: 10.1101/2020.03.27.20045153
- Liu W, Liu L, Kou G, Zheng Y, et al. Evaluation of nucleocapsid and spike protein-based ELISAs for detecting antibodies against SARS-CoV-2. medxriv [Internet]. 2020; Available from: https://doi.org/10.1101/2020.03.16.20035014 medRxiv preprint
- Unity Studies: Early Investigation Protocols https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/early-investigations
WHO continues to monitor the situation closely for any changes that may affect this interim guidance. Should any factors change, WHO will issue an update. Otherwise, this scientific brief will expire 1 year after the date of publication.